What Is A Service Plan In Health Care
Introduction
The structure of health services in the UK after the second world war reflected disparate origins and artificial divisions between different elements, which had persisted for many years. The 3 principal strands, state endemic (nationalised) hospitals, a national network of general practitioners and customs and domiciliary health services, were financed centrally but managed separately. Throughout the history of the NHS, this initial division of functions betwixt split statutory organisations created problems in the provision of comprehensive and co-ordinated services.nA report published in 1956 (Guillebaud Report), expressed early business organization almost many issues, which is nonetheless familiar.
These included:
- Irresolute trends in wellness and disease.
- The importance of prevention of illness.
- The needs for GPs and hospitals to work closely together.
- The need to make adequate provision for the intendance of erstwhile people Whether the NHS would in practise exist able to run across every demand justifiable on medical grounds.
The health and social intendance system continues to confront significant challenges of the future including:
Rising expectations: the public wanting more from their public services, to match the choice, customer service and personalisation they get elsewhere, and wanting services to be more local and convenient too.
The demographic challenge: with an ageing population and increasing numbers of people with long-term atmospheric condition including serious disabilities, increasing demand.
The revolution in medical technology: transforming the ability of the NHS to forestall, cure and manage diseases, alleviate suffering and extend life expectancy, but this creates new costs
Continuing variations in the prophylactic and quality of intendance: needing an NHS that delivers intendance of the highest possible safety and quality in every place and at every fourth dimension, in detail through honest and open information nigh the outcomes accomplished by providers.
Health Service Planning
'Health services planning' is a common term. It reflects the growing interest in the topic in the 21st century. The term tin can mean dissimilar things to unlike people, i.e. a notion of social applied science applied to healthcare or the design of a health
facility.
'Health services planning' has been described as:
A process that appraises the overall health needs of a geographic area or population and determines how these needs tin be met in the most effective way through the allotment of existing and anticipated time to come resources (Thomas 2003:3).
Ultimately, all planning comes down to identifying the needs of the target population and so determining the best means for meeting those needs. However, within the health sector in that location is uniqueness well-nigh the planning process that doesn't occur inside industry. This includes:
- Emotional dimensions - fluctuations in demand and the fact that health service providers are oftentimes dealing with life-and-death situations.
- Complex relationships - the healthcare manufacture is too made of many separate entities operating in a nearly uncoordinated mode and frequently at cross-purposes and characterised by a variety of different customers.
- Financial characteristics – different from other industries whereby the end-user may not brand the consumption decision or pay for the service provided
- Diversity of functions – different entities perform different functions and single entities, eastward.chiliad. a hospital, performs multiple functions simultaneously. The functions can range from, providing for the healthcare needs of a population to providing a community service and others seeing their role equally humanitarian or seeing themselves as contributing to the prophylactic of the public.
Health care needs vary co-ordinate to the age structure and wellness contour in a population. The likelihood of people seeking intendance is adamant past a range of social and cultural factors and will impact upon demand for care. The likelihood of people receiving care is determined by policy decisions and will impact upon the volume of activity in the health system.
Planning activities and terms
There are many planning terms, which need to exist understood in order to clarify the relationship betwixt these planning approaches. A summary of these terms is given below:
| Terms | Activity |
| Economic/development planning | National level activeness aimed at steering the economic or evolution policies, primarily though public expenditure or fiscal policies |
| Strategic programme | Document outlining the management an organisation is intending to follow, with wide guidance equally to the implications for services or activity |
| Business plan | Strategic plans prepared by business organisations setting out their direction, and normally providing income and expenditure projections |
| Regulatory planning | Activities of Country planning bodies that set planning guidelines for private sector activities |
| Service/plan planning | Planning focusing on the services to be provided. Used to contrast with capital planning (run across below) |
| Upper-case letter planning | Planning focusing on the majuscule developments of an system such every bit its building program |
| Project planning | Planning focusing on discrete time-limited activities |
| Man resources/manpower planning | Plans focusing on the human resource requirements of an organisation or country |
| Physical plans | Plans relating to structure elements |
| Operational plans | Activity plans detailing precise timing and mode of implementation |
| Work plans | Operational plans referring to the activities of a small unit or of an individual |
(Greenish 2007.49)
Initiating Health Services Planning
There are many reasons for initiating a health services planning process, which can emerge from, the community, an organisation or the interest of a particular group or individual. Nevertheless, any healthcare services program is going to reflect the influence of the political, social and economic considerations that are within that detail healthcare environs. Health service planning tin therefore exist undertaken on the basis of change arising from:
- healthcare reforms which inverse accountability and conclusion making inside the NHS
- health intendance needs which tin can change over time according to the age structure and health contour in a population; e.thousand. the increasing numbers of older people hateful a concomitant increase in inability and disease, in particular those of dementia, musculoskeletal and cardiovascular diseases, and sensory impairment. Wellness and social systems need to address the treatment and care of the increasing numbers of people with these problems.
- technological advances which continuously challenge the wellness service. Technology and medical advances are major drivers of health expenditure and have significant potential to improve the outcomes and the efficiency of the health service.
- evidence-base programmes setting quality standards and specifying services, e.grand. Dainty recommendations and qulity standards.
The challenge for the planner is to balance the objective, technical dimension of planning with the realities of the context within which the planning is taking place.
Planning approaches
There are diverse different approaches to health service planning which can range from 'problem solving', 'long-term versus shorter operational plans' and 'narrative approaches' which uses matrices presenting a nested prepare of objectives set in tabular course. Plans may also be aimed at detail services or institutions or at wider geographical areas.
Inside health planning there are two broad types:
- activity planning – is concerned with the maintenance of existing situations and the setting of monitorable implementation timetables.
- allocative planning – is concerned with the possibility of change and the making of decisions on how resources will be used and which activities will be undertaken.
The outcome of planning is conditioned past the behaviour of individuals and groups at all levels in the process. The NHS planning system is an enabling mechanism, which should facilitate a more effective utilize of the scarce resources available for wellness care.
Concerns about planning
The history of planning in the health sector is however relatively short and has non always been successful. The dilemma that gives rise to the needs for planning is often the gap between bachelor resources and health needs, leading to the requirement to make choices as to how to use these resource. Plans frequently fail to be implemented or are implemented but neglect to respond adequately to the real needs of the populations. Common examples are the imbalance of resources betwixt preventive care andcurative care, between different social groups, betwixt different regions orgeographical areas, between staff salaries and medical supplies, or betwixt different types of staff such as generalists and specialists. If planning is to exist strengthened in the future information technology is important to understand the reasons for any of these occurrences. A diversity of reasons can contribute to poor planning processes and include:
- planning becomes an cease in itself, with the real aim, that of effecting change – submerged nether the planning process
- technical failure to analyse needs appropriately or to estimate resource accurately
- imposing plans from the eye in a pinnacle-downwardly mode, without the involvement of both the wellness-intendance providers and the communities in the decision
- the planning process has been isolated from other conclusion-making processes such as budgeting or human being resource planning
- the failure to consider the inherently political nature of the process.
NHS reforms have encouraged a patient-led NHS that uses available resources as effectively and fairly as possible to promote health, reduce wellness inequalities and deliver the best and safest possible healthcare.
Planning Mechanisms and Techniques
Joint Strategic Needs Cess: In England The Local Government and Public
Involvement in Health Human action (2007) also specified that local regime and partners produce a Articulation Strategic Needs Cess (JSNA) of the wellness and wellbeing of the local customs. Needs assessment is an essential tool for commissioners to inform service planning and commissioning strategies. The findings of the JSNA should inform a number of local plans.
The stages in preparation of a JSNA volition include:
- stakeholder involvement
- engaging with communities
- suggestions on timing and linking with other strategic plans
- development of a core dataset.
Guidance on utilising JSNA to provide insight into local commissioning, publishing and feedback tin can be plant at
(http://webarchive.nationalarchives.gov.uk/20130105031054/http://world wide web.dh.gov.britain/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_081267.pdf )
The JSNA provides a framework to examine all the factors that impact on health and wellbeing of local communities, including employment, education, housing, and environmental factors. Local authorities and PCTs can build on this core dataset, using clearly defined criteria to select additional, high quality and locally relevant information that provides a clear motion picture of their area.
Undertaking Health Service Planning
Who is involved?
Planning is concerned with change and the prospect of change inevitably brings opponents and supporters of the proposal. The human relationship between planners, policy makers, service-managers, communities and other stakeholders in the planning procedure is critical to the success of planning. A significant number of health planners are fatigued from health professions, e.thousand. medicine, nursing, and public wellness, nonetheless i of the challenges today is non then much a matter of trying to develop specialist health planners but rather that of exposing a broad range of professionals to the importance and concepts of planning in gild that they can participate in the procedure. A second claiming is to ensure that planning systems are designed and operated and then as to provide real (rather than token) input from communities and users in the planning process.
Many techniques are used to assess the importance of stakeholders' influence including stakeholder assay (see Theories of strategic planning).
What is involved?
The following diagram represents a cyclical ready of activities frequently constitute during a planning process. It tin exist described as a planning spiral, with the cease bespeak of each bike forming the first of the next cycle, but at a higher plane.
The Planning Screw (Green 2007:36)
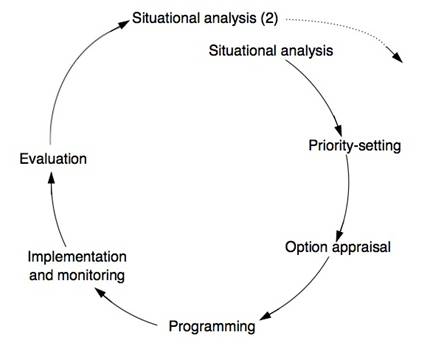
Each stage is briefly described beneath with links to examples in the field.
Situational analysis: involves assessing the present state of affairs and
includes:
- electric current and projected demographic characteristics of the population
- physical and socio-economic characteristics of the expanse and its infrastructure
- analysis of the policy and political surround including existing health policies
- analysis of the health needs of the population
- services provided by non-health sector every bit well as health sector, focusing on facilities provided, their function and service gaps together with organisational arrangements
- exam of resources in the provision of services including their electric current efficiency, effectiveness, equity and quality
The situational assay needs to cover the whole of the health sector.
Priority-setting: stage ensures that the priorities ready are feasible inside the social and political climate and within the context of bachelor resources. Clear criteria are therefore required for the selection of priority bug, which reflect the goals, objectives and targets of the organisations involved. In some situations information technology may exist helpful to clarify first what are non priorities (e.g. where local needs are low, where expectations cannot be met or meaning achievements have been made and needs are now less pressing.
Option appraisement: stage involves the generation and assessment of the various alternative strategies for achieving the prepare of objectives and targets. Options may exist discarded at this stage due to high resource implications, political or social unacceptability, or technical unfeasibility. The results of this stage will exist a list of preferred strategies or combination of approaches which will and so grade part of the plan.
Programming budgeting: Programme Budgeting (Lead) is an appraisal of past resources allocation in specified programmes, with a view to tracking future resource allocation in those same programmes. In addition, Marginal Analysis (MA) is the appraisal of the added benefits and added costs of a proposed investment (or the lost benefits and lower costs of a proposed disinvestment. Together PBMA is a priority-setting framework that helps conclusion-makers maximise the impact of healthcare resources on the wellness needs of a local population.
Example: PBMA in eight steps (Brambleby and Fordham):
- Step 1: Cull a set of meaningful programmes with which to work
- Step two: Identify current activity and expenditure in those programmes
- Step iii: Be creative – consider possibilities for improvements and linkages in pathways and patterns of intendance inside and between programmes
- Step 4: Weigh up extra costs and increased benefits of the improvements that were thought of in Stride 3
- Stride 5: Consult widely – there may exist options, trade-offs and value judgements to explain
- Step 6: Decide on the change and make the conclusion in public
- Step 7: Event the change – this is the essence of management – making information technology happen
- Step 8: Evaluate your progress – cheque that the anticipated costs, saving and outcomes actually materialised.
To notice examples from these steps see (http://www.bandolier.org.uk/painres/download/whatis/pbma.pdf)
Implementation and monitoring: is an essential part of the planning procedure which involves transforming the wide strategies and programmes into more specific timed and approaching set up of tasks and activities and involves drawing upwards more operational plans which tin can then be monitored.
Evaluation: provides the basis for the next situation analysis and is an integral component of the process. Reflection upon whether the procedure has enhanced articulation working, the needs analysis has been sufficiently appropriate and comprehensive and if there are any gaps or areas of business concern that need farther analysis.
Using the Planning Spiral can brings all aspects of planning into a coherent, unified procedure.
References
- Department of Health (2002) Delivering the NHS Plan next steps on investment next steps on reform London: Crown
- Department of Health (2008) Joint Strategic Needs Assessment Quality Assurance Toolkit NHS Eastward of England
- Green, A. (2007) An Introduction to wellness planning for developing health systems Oxford University Press
- Greengross, P.; Grant, 1000.; Collin. Due east. (1999) The history and development of the UK National Wellness Service 1948 – 1999 HSRC
- Ham, C (1999) Improving NHS performance: human being behaviour and wellness policy
British Medical Journal 319(7223): 14990-1492 - Mitton, C. and Donaldson, C. (2004) Priority Setting Toolkit A Guide to the Utilize of Economic science in Healthcare Decision Making London: BMJ Publishing
- Pencheon, D.; Guest, C.; Melzer, D.; and Gray, Chiliad.J.A. (2006) Oxford Handbook of Public Wellness Exercise Oxford University Press
- Rathwell, T. (1987) Strategic Planning in the health sector Kent: Croome Helme
- Thomas, R.Grand. (2003) Health Services Planning New York: Kluwer Academic Publishers
© S Markwell 2009, C Beynon 2017
What Is A Service Plan In Health Care,
Source: https://www.healthknowledge.org.uk/public-health-textbook/organisation-management/5d-theory-process-strategy-development/health-service-development-planning
Posted by: watsoncautity.blogspot.com


0 Response to "What Is A Service Plan In Health Care"
Post a Comment